Achalasia
What is Achalasia?
Achalasia is an esophageal disease that inhibits normal esophageal emptying. In patients with Achalasia, specific esophageal nerve fibers are damaged. The esophagus loses its capacity to push, and the valve at the lower end of the esophagus (also known as the lower esophageal sphincter) does not relax adequately, leading to difficulties swallowing and a number of accompanying symptoms. Achalasia is in many respects the opposite of GERD, but often patients have similar “heartburn” symptoms so are treated for GERD for many years before the correct diagnosis is made. Achalasia patients have an abnormally tight lower esophageal sphincter, whereas GERD patients have a weaker lower esophageal sphincter. Both illnesses can have a significant influence on a patient’s quality of life and, if left untreated, can result in more serious health problems.
Achalasia, like GERD, can occur at any age, but is more prevalent in middle-aged and older people. It affects men and women equally, and no specific causes have been identified.

Symptoms of Achalasia
Achalasia patients may experience any number of symptoms, however the following are the most common:
How to Diagnose Achalasia
There are two primary diagnostic tests used to identify Achalasia. These are essential for determining which subtype of achalasia a patient has, which has a significant impact on the treatment regimen.
Treatment of Achalasia
There are multiple therapeutic options available to minimize the symptoms of Achalasia, but Achalasia is a lifelong illness for which there is presently no “cure”. No intervention will be able to restore the motility of the esophagus to its normal state. All interventions are directed at decreasing the barrier caused by the tight lower esophageal sphincter in order to allow easier passage of liquids and solids into the stomach.
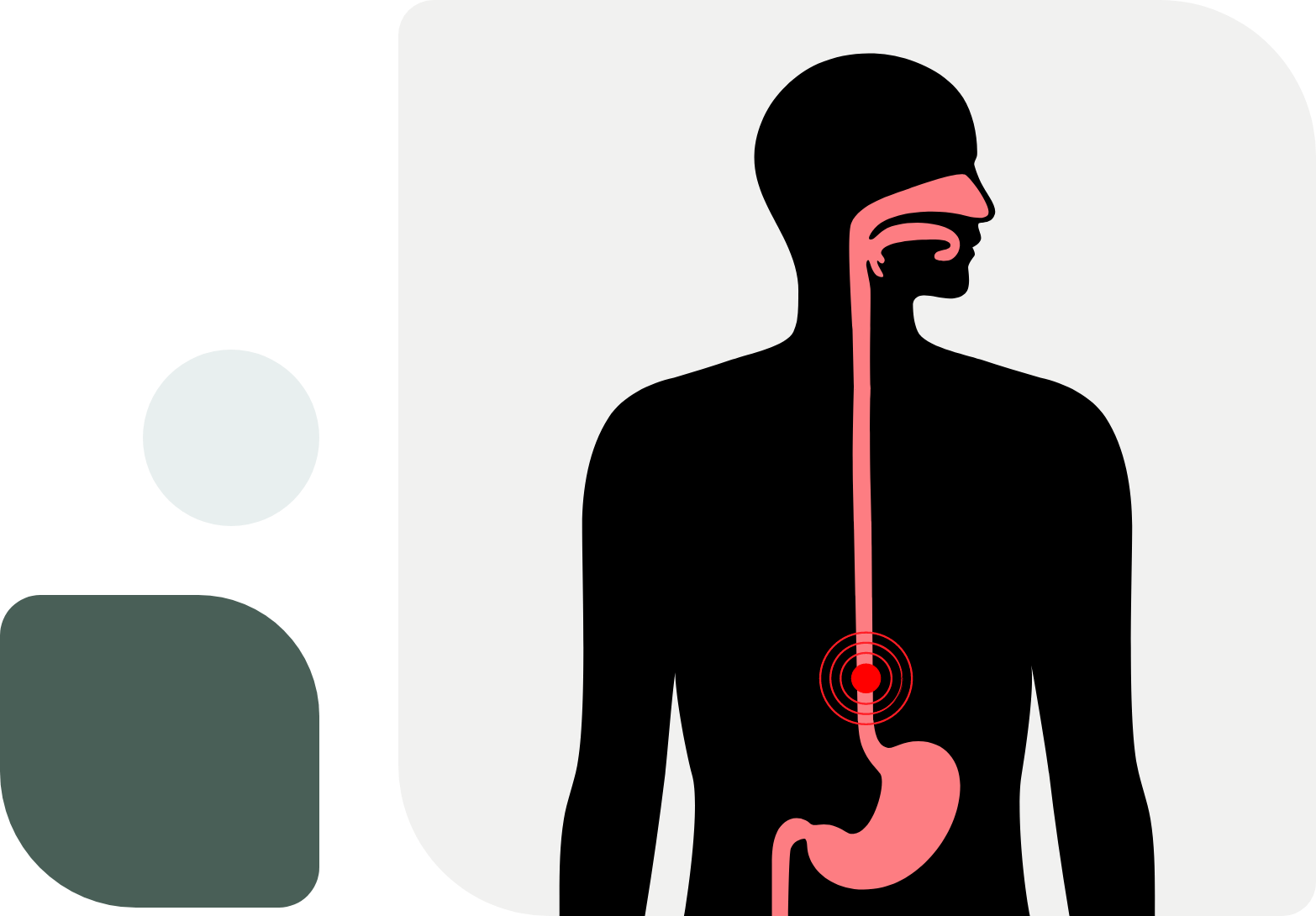
The most common operation used to treat Achalasia is the robotic Heller myotomy, a robotic procedure involving the severing of the LES muscle to alleviate difficulty swallowing, allow food and liquids to flow into the stomach. During the process, the LES is partially reconstructed to prevent severe reflux after surgery. Surgery has proven to be the most effective long-term treatment for Achalasia, and the majority of patients see almost immediate improvement in swallowing function.
Another procedure that can be used to treat Achalasia is the POEM or PerOral Endoscopic Myotomy. This procedure is performed completely endoscopically. In certain subtypes of achalasia, the POEM procedure is very effective at treating patients symptoms. It does come with some increased reflux compared to a Heller myotomy. If after testing and discussion with patients that are good candidate for the POEM procedure, Dr. Grandhige will refer them to a specific physician in the Tampa area who specializes in this form of therapy.
